Toe walking: causes, epidemiology, assessment, and treatment
Joseph J. Ruzbarsky, David Scher, and Emily Dodwell
Curr Opin Pediatr 2016, 28:40-46
Key points
l Toe walking can be related to structural abnormalities such as tendon contracture or leg length discrepancy, or neurologic/neuromuscular conditions such as autism, cerebral palsy, or muscular dystrophy.
l Most cases of toe walking are idiopathic, without a discernable underlying cause.
l Physical therapy, orthotics, serial casting, chemical denervation, and surgical lengthening of the gastroc–soleus–Achilles complex are described treatment options.
l Treatment for toe walking is based on age, underlying cause, and the severity of tendon contracture.
l Recent systematic reviews show good evidence for the use of casting and surgery, with surgical interventions showing the most promising long term results.
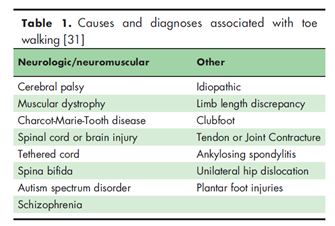
까치발 보행(toe walking, Fig.1)은 보행의 입각기 시작을 발뒤꿈치 딛기 대신 발가락이나 전족부로 딛는 것으로, 보행 발달 측면에서 정상적으로 나타날 수 있으나 3-7세 사이에 소실되어야 한다. 그렇지 않을 경우에는 힘줄 구축, 짧은 다리의 보상, 자폐 스펙트럼 장애의 징후, 뇌성마비, 근이영양증, 혹은 다른 신경, 신경근 질환의 증상일 수 있다(Table 1). 특발성 까치발 보행(Idiopathic toe walking, IWT)의 진단은 다른 가능성이 있는 진단이 모두 배제되었을 때 가능하다. 까치발 보행은 단순 외형적인 문제일 수도 있지만 발이나 발목의 통증을 유발하고 보상성 보행 이상으로 에너지 소모를 증가시키고 환아나 가족에게 정신적인 고충을 가져온다. 유병율은 5.5세를 기준으로 정상 발달 환아의 2%, 신경정신학적 혹은 발달 지연을 보이는 환아의 41%이며 남아에서 많이 발생하는 경향이 있다. 관절의 유연성은 초기에는 정상적이나 시간이 지나면서 gastroc-soleus complex의 과도한 사용과 plantarflexion 자세의 지속으로 족관절 배굴이 제한된다. 특발성 까치발 보행의 경우에는 환아가 습관적으로 까치발 자세를 취하지만 바른 자세를 요구하면 발뒤꿈치 딛기를 자발적으로 할 수 있다. 이 전에는 특발성 까치발 보행이 단순히 습관이나 좋아하는 자세라고 생각되었지만 정상적인 보행을 하는 청소년과 비교했을 때 운동 조절, 감각 처리, 진동 감각 역치의 차이를 동반하는 언어 발달 지연, 실행 능력, 사회적 기능, 학습, 기억 능력의 이상을 보이는 것과 관련이 있는 경우가 종종 관찰되었고 세포 수준에서는 Type 1 muscle fiber의 농도 증가가 관찰되고 10~88%에서는 상염색체 우성 유전을 보이는 가족력이 있다. 특발성 까치발 보행의 코호트 연구에서 3년 정도 관찰했을 때 12%정도만이 까치발 보행을 중단하였다. 시간이 지나면서 중족부에 가해지는 압력의 증가로 foot pain, callouses, stress fracture, difficulty with shoe wear 와 같은 문제가 발생한다. 주의 깊은 병력 청취, 이학적 검사, 진단학적 검사가 타입을 분류하고 적절한 치료를 결정하는데 중요하다고 하겠다.

1. 병력 청취
가족의 관심 부분, 기능상의 문제, 통증의 유무, 사회적 기능의 문제, 외형적인 문제, 출생과 발달 문제, 발생 시점, 발뒤꿈치 딛기 가능 여부, 내과적, 외과적 과거력, 가족력, 치료 경험 등을 자세히 확인하여야한다.
2. 진찰
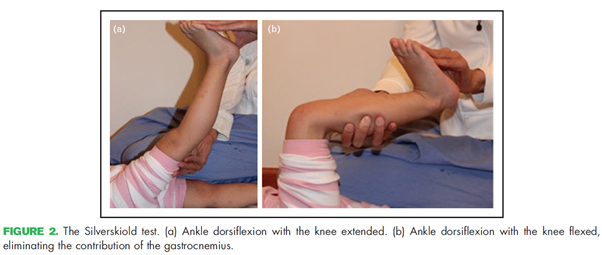
아이가 진료실에 걸어 들어오기까지 관찰을 하자. 맨발과 신발을 신은 상태에서 발뒤꿈치를 땅에 닿도록 노력하면서 자연스럽게 보행을 하도록 하고 사방에서 보행 양상을 확인한다. 입각기에 equinus의 정도, 유각기에 배굴이 적절한지, 무릎과 고관절의 움직임, 까치발 보행을 한쪽으로 만 하는지, 상지의 움직임은 정상적인지, 서있는 자세에서 발뒤꿈치가 땅에 닿는지, 다리 길이 차이는 없는지, 근위축은 없는지 등을 관찰한다. Silverskiold test (Fig. 2)를 시행하여 배굴이 안되는 것이 gastrocnemius tightness 만의 문제인지, soleus tightness 와 동반된 문제인지 구별할 수 있다. 피부의 callouses or erythema 여부, 신발이 닳는 패턴을 확인하는 것도 중요하다. Full neurologic exam을 시행하여 다른 신경학적 질환과 근육병 등을 배제하는 것이 중요하고 신경학적 검사가 정상적이더라도 3-5년 이상의 까치발 보행을 보였다면 신경과 의사에게 의뢰해 다른 문제를 확인하는 것이 필요하다.
3. 진단적 검사
Lab(CPK), Imaging(rigid equinus deformity), 보행 분석, EMG(GCM의 early firing이 IWT와 diplegic cerebral palsy 둘다에서 관찰되지만 knee extension 상태에서 GCM coactivation은 뇌성마비에서 더 많이 관찰되는 경향이 있음), Brain and spinal MRI 검사 등이 다른 질환을 배제하기 위해 필요하다.
4. 치료 – IDIOPATHIC TOE WALKING
Cueing, physical therapy & stretching, Botox 는 관찰하며 지켜보는 것 보다 뛰어나다는 증거가 불명확하다. Rigid inserts와 AFO는 단독으로 큰 효과가 없으며 AFO는 수술 후 상태에서 도움을 준다. 5세 이하에서는 이러한 보존적인 방법들을 적절하게 case에 맞게 적용하면서 자연적으로 소실되는지를 관찰한다. 하지만 5세 이상에서도 지속될 경우에는 Casting을 적용해 볼 수 있으며, 배굴이 10도 이상 나올 경우 6주 동안 최대한 배굴 각도로 고정해서 casting을 시행함으로써 습관을 교정해 볼 수 있고, 배굴이 10 도 이하에서 제한되어 있을 경우에는 매 1-2주 마다 casting을 바꾸면서 최대한의 배굴 각도를 회복할 수 있다. 하지만 7세가 넘으면 casting은 크게 효과가 없고 배굴이 neutral을 회복하지 못하면 수술적 치료를 고려해야 한다.
5. 치료 – AUTISM SPECTRUM DISORDERS
ITW의 치료 알고리즘과 비슷하게 시도해 볼 수 있으나 인지 저하, 감각 이상 등의 문제로 치료에 잘 반응하지 않으므로 통증이나 기능적인 문제가 크게 문제 되지 않으면 지켜 보는 것이 우선이고 구축이 발생할 경우에는 수술 치료 후 AFO를 착용하여 재발을 방지 할 수 있다.
6. 결론
까치발 보행은 기저 질환과 연관이 있을 수 있지만 대부분의 경우 특발성 까치발 보행으로 병력 청취, 이학적 검사, 진단적 검사를 시행하여 원인을 확인 후 질환을 배제하는 것이 필요하며 치료 방법으로 현재까지는 serial casting과 surgical lengthening이 가장 효과적인 것으로 밝혀져 있으나 향후 전향적인 비교 연구가 필요한 상태이다.